Congestive Heart Failure
- Zach Atwood
- Mar 7, 2021
- 5 min read
Description
Heart failure is a complex clinical syndrome that results from any functional or structural heart disorder, impairing ventricular filling or ejection of blood to the systemic circulation to meet the systemic needs. Heart failure can be caused by diseases of the endocardium, myocardium, pericardium, heart valves, vessels, or metabolic disorders. Most patients with Heart failure have symptoms due to impaired left ventricular myocardial function. Patients usually present with symptoms of dyspnea, decreased exercise tolerance, and fluid retention, characterized by pulmonary and peripheral edema (1).
Heart failure due to left ventricular dysfunction is categorized according to left ventricular ejection fraction (LVEF) into heart failure with reduced ejection fraction usually <40% (1).

Etiology
Approximately 5.1 million people in the United States have clinically manifest heart failure, and the prevalence continues to increase. Heart failure incidence has remained stable over the past decades, with more than 650,000 new cases of heart failure cases diagnosed annually, especially for individuals greater than 65 years of age (1).
Black men have the highest incidence rate (1000 person-years) for heart failure and the greatest five-year mortality rate when compared to whites. White women represent the lowest incidence. Heart failure in non-Hispanic black males and females has a prevalence of 4.5% and 3.8%, respectively, versus 2.7% and 1.8% in non-Hispanic white males and females, respectively (1).
Heart failure is caused by several disorders, including diseases affecting the pericardium, myocardium, endocardium, cardiac valves, vasculature, or metabolism (1).
The most common causes of systolic dysfunction HFrEF (heart rate with reduced ejection fraction) are idiopathic dilated cardiomyopathy (DCM), coronary heart disease (ischemic), hypertension, and valvular disease (1).
Gender differences in heart failure:
Between ages 65-85, heart failure incidence doubles in men but at the same time, it triples in women.
Women are likely to have preserved systolic function compared to men.
Women, in general, develop heart failure later in life compared to men.
While the symptoms of heart failure are similar in both genders, they are often severe in females.
Women with heart failure tend to have longer survival times compared to men (1).
Pathogenesis
Left-sided heart failure
Decreased pumping of the left ventricle leads to ventricular dilation as compensation for greater volumes of blood. This increased volume puts an excessive stretch on the L ventricular wall. When it is stretched beyond a certain point, also known as a poor length-tension relationship, the contraction becomes inefficient. Meanwhile, the right ventricle continues to pump blood to the lungs, which leads to pulmonary congestion because the left ventricle is not able to meet the demands of pumping blood to the rest of the body.
The sympathetic nervous system is activated, increasing heart rate and muscle mass (hypertrophy) to help compensate. However, there is not enough O2 to meet the demands of the enlarged heart which can lead to angina (chest pain due to lack of blood flow to the heart).
The Renin-Angiotensin-Aldosterone system is activated as a result of less blood flow going to the kidneys, This causes vasoconstriction in the periphery, which increases the afterload, putting more demand on the heart. Less blood getting to the kidneys leads to more water retainment causing edema and therefore increasing the preload on the heart (4).
Right-sided heart failure
The number one cause of right-sided heart failure is left-sided heart failure. The blood gets backed up and is then shunted to the periphery. Pure right-sided heart failure can be due to Cor pulmonale.
The pathophysiology of cor pulmonale is a result of increased right-sided filling pressures from pulmonary hypertension that is associated with diseases of the lung (2).
The initial pathophysiologic event in the production of cor pulmonale is an elevation of pulmonary vascular resistance. As the resistance increases, the pulmonary arterial pressure rises, and the right ventricular work increases leading to right ventricular enlargement (e.g., thickening, dilation, or both) (2).
Clinical Presentation
Left-sided:
Fatigue & Dyspnea with mild exertion.
Paroxysmal Nocturnal Dyspnea: SOB and difficulty breathing at night. Feels like drowning in their own fluid.
Orthopnea: SOB while laying flat.
Persistent spasmodic cough especially when lying down.
Pulmonary crackles.
Tachycardia.
Muscle weakness.
Dry cough or cough with pink frothy sputum.
Edema and weight gain (>2-3 lbs day).
Irritability/restlessness.
Decreased renal function (frequent urination at night due to improved blood flow to the kidneys in a recumbent position).
Heart sounds: S3 gallop (Lub du dub): a low-pitched sound that results from a large amount of blood hitting a very compliant (dilated) left ventricle.
Abnormal pulse pressure (predicts mortality): pulse pressure is the difference between systolic and diastolic blood pressure (4).
Right-sided:
Increased fatigue.
Dependent edema (usually beginning in the ankles).
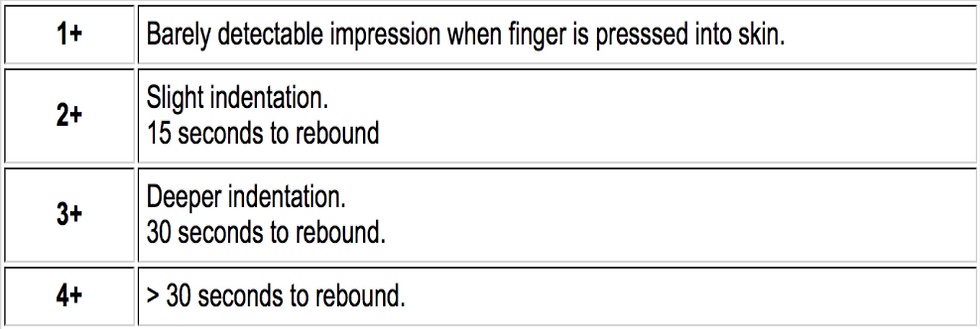
Pitting edema (5-10 lbs of fluid).
Edema in sacral area or back of thighs.
Right jugular venous distention (>3-4 cm).

Early satiety, nausea, and vomiting, or abdominal discomfort.
Cyanosis (4).

Pitting Edema Scale
CHF –New York Heat Association Functional Classification

Diagnosis
Chest x-ray: will show an increased size of the heart, potentially the presence of fluid in the lungs, and possibly atelectasis (collapsed lung).

Echocardiogram: will reveal ejection fraction, the size of the ventricles, and thickness of the ventricular wall.
ECG may reveal underlying causes such as infarctions or arrhythmias.
Laboratory tests: Patients may have elevated creatinine and BUN (blood urea nitrogen). Sometimes, PaO2 and O2 sat can be decreased. Liver enzymes can be elevated. BNP (B-type natriuretic peptide) >700 indicative of heart failure (4).
Progression of CHF
Cardia Pump Dysfunction
EF >30%-50%.
Abnormal heart rate response.
Functional capacity 5-6 METS.
Hypertensive BP response.
Non-malignant arrhythmias (3).
Cardiac Pump Failure
EF <30%.
Abnormal heart rate response.
Functional Capacity 4-5 METS.
Flat or falling blood pressure response.
Complex ventricular arrhythmias.
Lower EF, lower the prognosis for CHF(3).
CHF PT Implications
Often have elevated HRs and low BP at rest.
Many exhibit chronotropic incompetence (failure to adequately increase HR during exertion).
EF less than 40% is more likely to exhibit abnormal responses to exercise; however, there is a poor correlation between EF and exercise tolerance.
Progress slowly and monitor carefully.
Frequent 1- to 2-minute rests.
Caution with supine or prone positions.
No Valsalva maneuver.
Long warm-ups and long cooldowns.
Drugs can cause orthostatic hypotension (4).
Signs and symptoms of fluid overload
Edema.
Rales/crackles.
S3 gallop.
Decreased tolerance to activities/fatigue.
Dyspnea.
Increased weight gain (4).
*Document any changes listed above
Recognizing CHF Exacerbation
The first thing to notice is a decreased tolerance to physical activity.
Patients with CHF need to weigh themselves every day at the same time to keep it consistent and document any changes.
Increased weight of 2-3 lbs in 24 hours or 4-6 lbs in 72 hours is very concerning.
A dry hacking cough may be accompanied by pink frothy sputum.
Early satiety, nausea, and vomiting, or abdominal discomfort.
Belt tighter or increased abdominal girth.
Decreased urination throughout the day.
Chest pain or heaviness.
Confusion or restlessness (4).
*Any of the above should result in referring back to the physician for a follow-up.
Board Questions
A 56-year-old patient presents to the clinic with a chief complaint of shortness of breath and fatigue while exercising, abdominal discomfort, and swelling in the LE's. Which of the following do you suspect to find upon objective examination?
S4 heart sound
Wheezing
S3 heart sound
Increased AP chest diameter
A 75-year-old male presents to the hospital with shortness of breath. Which of the following lab values will help rule in the diagnosis of heart failure?
Hemoglobin: 15.1 g/dL
Creatine: 1.0 mg/dL
BNP: 700 pg/mL
Hematocrit: 45%
Answers:
S3 heart sound is the correct answer for question number one. S4 is common L ventricular hypertrophy as a result of chronic hypertension. S3 is common in a dilated L ventricle and is the sound caused by the blood splashing up against the compliant ventricular wall. Wheezing is not common in CHF, crackles are often heard from the fluid built up in the lungs. Increased AP diameter is not a common sign in CHF, rather more common in COPD.
A BNP of 700 pg/mL would help you rule in the diagnosis of CHF. The higher the BNP, the lower the prognosis for CHF is. The higher the number indicates heart failure. Normal is less than 100. Creatine, hematocrit, and hemoglobin are all normal in this individual.
References
Malik A, Brito D, Chhabra L. Congestive Heart Failure. [Updated 2021 Feb 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430873/
Garrison DM, Pendela VS, Memon J. Cor Pulmonale. [Updated 2020 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430739/
Cardiovascular and Pulmonary Physical Therapy, Deturk and Cahalin, 2004
Goodman, Implications for the physical therapist. 4th edition.


.png)



Comments